
Autoimmunity: A Mystery Unsolved (Part 1)
Autoimmune diseases have long puzzled both doctors and patients. They occur when the body’s immune system, designed to protect us from invaders like bacteria and viruses, mistakenly attacks its own cells. It’s as if our internal defense system has gone rogue, waging a war against us. But why does this happen? The answer isn’t simple—it involves a combination of factors, including genetics, environment, and one increasingly understood trigger: the gut.
What Triggers Autoimmunity?
Autoimmunity doesn’t have just one cause—it’s the result of multiple factors that push the immune system into overdrive. Some common triggers include:
Genetic predisposition: A family history of autoimmune diseases makes some individuals more susceptible.
Environmental toxins: Chemicals, pollution, and pesticides can stress the immune system.
Infections and viruses: Certain infections confuse the immune system, causing it to attack the body’s tissues.
Chronic stress: Prolonged stress heightens the risk of immune system dysregulation.
Hormonal imbalances: Shifts in hormones, especially during pregnancy or menopause, can trigger or exacerbate autoimmune conditions.
Medications: Long-term use of certain medications can compromise immune regulation, leading to autoimmunity.
While all of these factors can contribute, one of the most compelling and emerging triggers is the leaky gut.
Leaky Gut: The Gateway to Autoimmunity
The gut acts like a selective barrier, allowing only essential nutrients to pass through while keeping out harmful substances. This is managed by the intestinal lining, which is often compared to a mesh or sieve. Under normal circumstances, this mesh is tightly regulated, ensuring that only selective particles like nutrients make their way into the bloodstream. However, due to factors like poor diet, stress, medications, and processed foods, this mesh can become compromised, leading to what’s known as leaky gut.
Here’s how the mechanism works:
- Gut Lining Damage: The tight junctions in the gut lining loosen due to various lifestyle factors, making the barrier less effective.
- Unwanted Particles Enter the Bloodstream: Normally, the gut only lets through nutrients, but when it’s compromised, large particles such as toxins, gluten, and casein sneak into the bloodstream.
- Immune system Reacts: These foreign invaders activate the immune system, which begins to produce antibodies to defend the body.
- Molecular Mimicry: Some of these foreign particles resemble the body’s own cells. The immune system, now confused, attacks not only the invaders but also healthy tissues that resemble these proteins.
- Autoimmune Response: This leads to a full-blown autoimmune attack, where the body mistakenly targets its own tissues, causing chronic inflammation and damage.
Molecular Mimicry in Action
One of the most intriguing aspects of autoimmunity is molecular mimicry, where proteins that pass through the gut barrier mimic the body’s own cells. This can lead to the immune system attacking specific organs or tissues:
- Psoriasis (Skin Cells): Proteins resembling skin cells slip through the gut and trigger an immune response, leading to the rapid turnover of skin cells and the characteristic scaly patches of psoriasis.
- Hashimoto’s Thyroiditis (Thyroid Cells): Gluten proteins, which can mimic thyroid cells, trick the immune system into attacking the thyroid, leading to hypothyroidism.
- Rheumatoid Arthritis (Joint Tissues): Viral or bacterial proteins can mimic proteins in the joints, leading to immune attacks on the synovial tissue, causing joint inflammation and pain.
- Multiple Sclerosis (Nerve Cells): Viral proteins that resemble the myelin sheath, the protective layer around nerve cells, cause the immune system to attack the myelin, disrupting nerve function.
Autoimmune diseases are becoming increasingly common, impacting millions of people worldwide. The complexity of these conditions makes them difficult to fully understand, but we now know that factors like genetics, environment, stress, and especially gut health play a major role in triggering them.
However, the story doesn’t end here. There’s growing evidence that our thoughts, emotions, and mental well-being can also influence the activation of autoimmune responses. In Part 2, we’ll dive deeper into the mind-body connection and explore how the way we think and feel can affect our immune system, sometimes for better, and sometimes for worse.
Stay Tuned!
- Lifestyle
- Nutrition
- Well-being

The Silent Decline: Why Men Are Losing Testosterone Faster Than Ever
There’s a quiet crisis playing out in men’s health and it has nothing to do with fitness trends or protein shakes. It’s testosterone. And it’s falling fast. Studies show that men today have 20-30% lower testosterone levels than men of the same age two decades ago. That’s not genetics, that’s lifestyle. Every year, the numbers […]
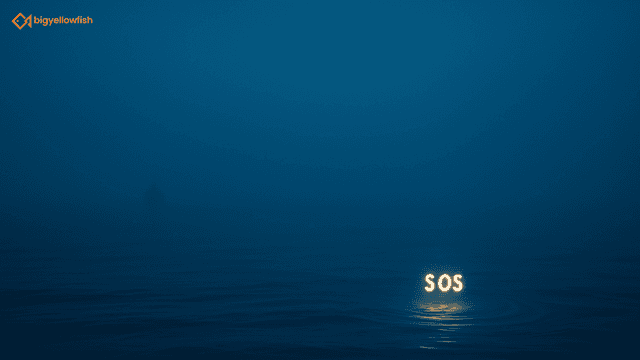
Invisible Emergencies
“Help. Help. Help. I am drowning.” “Maybe we can come back tomorrow to rescue this poor lad… I’m sure they can hang in a little longer…” said no one ever. Because physical injury is visible. The need for repair seems obvious. It’s instinctual to identify a human in crisis — an accident, a burn, a […]

 Workplace Well-being
Workplace Well-being Reinforced Learning
Reinforced Learning Collaboration
Collaboration